BioE Students Shine in Senior Design

Dr. Jennifer Amos, Bioengineering Chief Academic Advisor
June 4, 2012
After several years of learning principles and how to apply what they had learned to come up with practical solutions for real-life problems, Bioengineering students were given the opportunity to do just that.
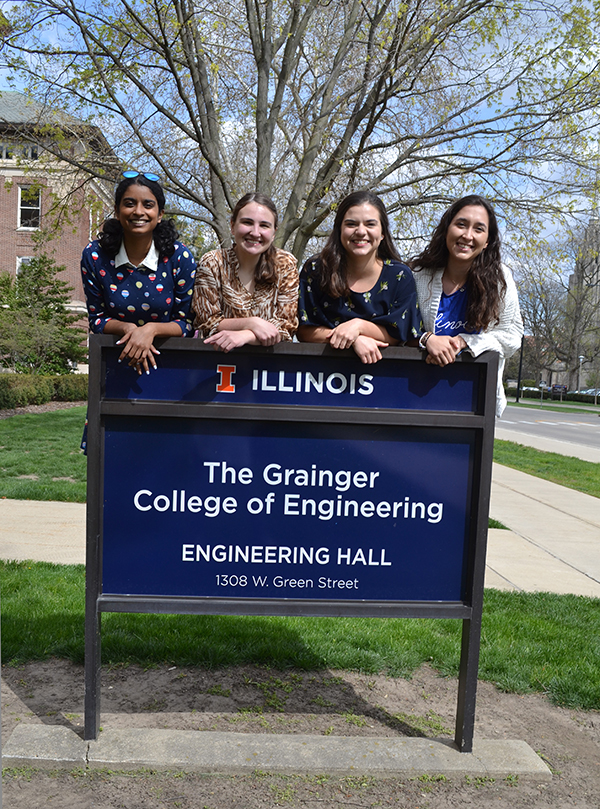
Sponsored by industry, university faculty, area medical clinics, and/or the community, Bioengineering seniors participating in this capstone design course over the past academic year completed projects that ranged from diagnosing cancer to designing a prothsesis that will enable below-elbow amputees to swim. Students were able to showcase their projects both during a formal presentation and a vendor fair at the end-of-the-year event which took place at NCSA on May 3, 2012, and was attended by family members, project sponsors, and university faculty and staff, including Dr. Jennifer Amos, Chief Academic Advisor in Bioengineering, who helped connect student teams with their sponsors and served as a major source of support for them throughout the year. Following are brief synopses of the various projects and what real-life problem areas they addressed.
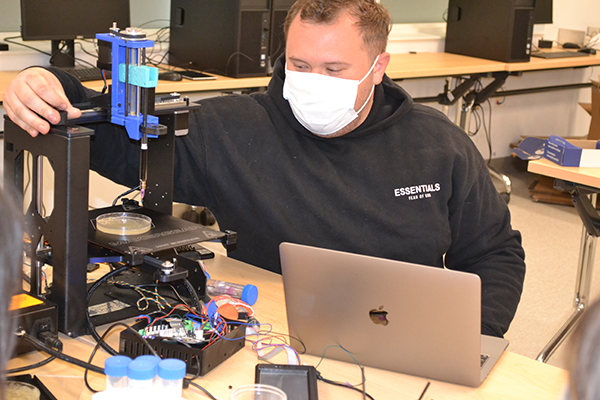
Working with Professor Rashid Bashir of Micro and Nanotechnology, Team Fish and Chips built a tool to help in the diagnosis of cancer, a Microfluidic Exosome Chamber. Nicknamed NanoCAMP (Nanoparticle Capture Microfluidic Platform), the device performs nanoparticle separation to isolate lyse exosomes, which cancer cells increase the excretion of exosomes compared to normal cells. The team demonstrated separation of two different sizes of cells, axioms and viruses and easily fabricated these devices in a chip format. Compared to other methods of separating it was fast and did not require bulky equipment to get the separation. The hand-held device that could be useful for third world diagnostic needs.
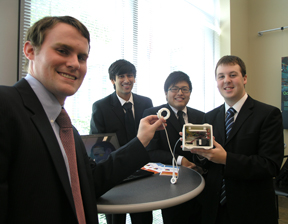
Team Real Solutions exhibits the blue-tooth-operated gastric band pump they designed.
Working with Dr. Uretz J. Oliphant, Interim Regional Dean of Medicine at Illinois, Team Real Solutions, in cooperation with a team from Mechanical Engineering, designed a blue-tooth-operated bidirectional pump to inflate/deflate a gastric band's pillows to adjust its fit. Currently, gastric band adjustments are done via a long needle inserted through layers of flesh and fat to add liquid to a fill port, which is not only uncomfortable, but expensive, since this procedure must be done several times a year, often with additional x-rays to find the fill port. Since the pump would be surgically implanted at the same time as the gastric band; compared to the current method, the pump is much less expensive, more efficient, and noninvasive.
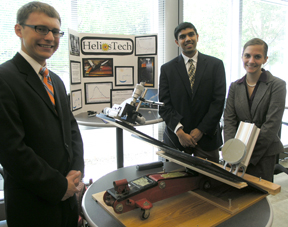
Team Helios Tech shows their solar-powered FOCT device for imaging the retina of the eye.

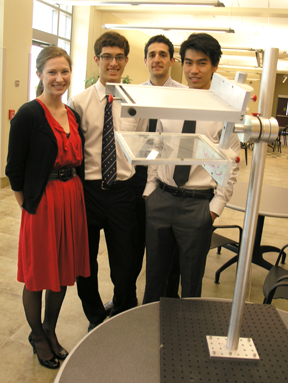
Team Streamline demonstrates the prosthesis they designed which will enable below-elbow amputees to swim.
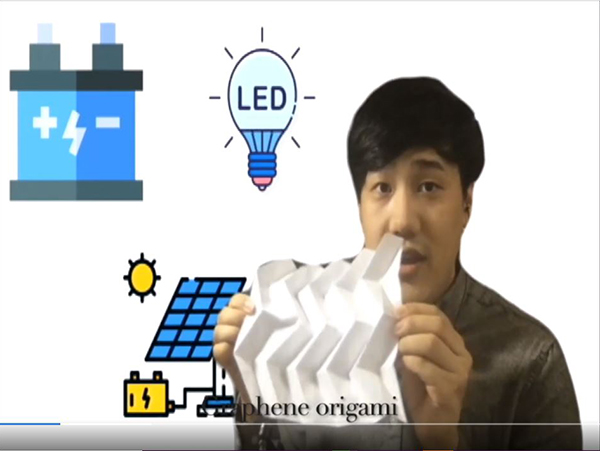
The Helios Tech Team, working with Dr. Steven Boppart in the Department of Electrical and Computer Engineering, and Bioengineering, created a device which captures light to power Optical Coherence Tomography (OCT), a non-invasive technology used for imaging the retina of the eye. While the traditional OCT is revolutionizing the early detection and treatment of eye conditions, because of the laser technology it uses, it is prohibitively expensive for underserved regions such as rural areas and undeveloped countries. This team developed an inexpensive, solar-powered system which uses a car jack to perform adjustments in order to capture more sunlight.
While amputees have at their disposal many specialized prosthetics designed to help them with daily tasks, nothing has been created that can mimic the motions a human arm makes while swimming…until now. Team Streamline, working with Dr. William Schuh, Medical Director at Carle, designed a device that performs a swimmers' stroke, thus enabling below-elbow amputees to swim.
Team Ramammogram shows the Raman Assisted Mammogram device they designed.
Team Ramammogram, working with Rohit Bhargava, Department of Bioengineering, worked to develop a new technology for diagnosing breast cancer, Raman Assisted Mammogram, which uses Raman spectroscopy rather than the ionizing radiation normally used in typical mammograms. Because of its superior imaging capabilities, Raman spectroscopy can distinguish between tissue types, especially when imaging dense breast tissue.
The two Ability One teams were sponsored by the Developmental Services Center (DSC) of Champaign, which works to provide services and supports to individuals with disabilities, including jobs such as sorting and bagging items for certain manufacturers. Team One created a magnetic part sorter which will enable the persons employed by the DSC to sort small parts and bag them without the need to count or pick up the items individually.

BioE students demonstrate the bag sorter they designed for the Developmental Services Center.
Also working with the DSC, Team Two working with Dr. Jennie Chung-Yi-Hsu-Lumetta of Internal Medicine, designed an assistive bagging chamber to help workers who sort items into plastic bags. Because the bags are difficult to hold open, the assistance of a supervisor has often been required to help get every new bag ready, which can be very time consuming. So Team Two created a device which holds a supply of bags and which the bagger can use to hold a bag open without the assistance of a supervisor. To operate the device, one pushes in on the lever to latch on to a new bag, then pulls the lever out, which holds the bag open the required width for inserting the items.
Despite our society's active population, in which joint injuries are becoming more common, there is currently no brace available that can actively assist the user to stand from a seated position, often needed during rehabilitation. However, Team Biodynamics has changed that. Working with Dr. Philbert Chen of Carle, they designed an active knee brace; it not only braces the knee, but has springs which assist the injured person to stand up from a seated position.

Students from Team Biodynamics showcase the active knee brace their team designed.
Also working with Dr. Chen, Team Snore No More developed a screening tool for sleep apnea. For example, persons who need the sleep apnea test, such as Truck drivers, who are required to take the tests before they can receive their license, often at an expensive sleep center. and A large market exists for portable cheap sleep apnea diagnosis and treatment machines for truck drivers. for many, it is an out of pocket cost at an expensive sleep center. This device will create an accurate system to diagnose quickly and affordably.

Team Illini Medical Models exhibits their deep laceration model. The inset shows the layers and how the model would be used to practice making stitches.
The Illini Medical Models team created a Deep Tissue Laceration Model. Because students studying medicine lack the tools to practice suturing, Dr. Estes from the University of Illinois College of Medicine in Peoria requisitioned a model on which medical students could practice. This team's students worked diligently to find materials that would simulate the simulate irregular edges, realistic skin, fat, connective tissues, muscle, and subcutaneous tissue that someone suturing a real deep tissue laceration would encounter, and then constructed the model from a variety of materials: PVC, silicon rubber, knit fabric, foam, and liquid latex.

Members of the Gout Busters Team demonstrate how a medical student would practice tapping fluid from the big toe of the model they created to test for gout.
In another model for use by medical students, the Team Gout Busters developed a model of a foot on which medical students could practice on to tap the synovial fluid of the big toe for analysis to determine if the patient had gout. Designed for Dr. Thomas Santoro at the University of Illinois College of Medicine at Peoria, the foot model required mobility of joints and a movable big toe, plus it needed to contain a liquid in the big toe joint that caused the person doing the procedure to feel a "pop" similar to what one feels when doing the procedure on a living joint, and had liquid that could be extracted. The life-like model of the human foot which the students designed (complete with a French manicure) had all of these mobility requirements and a renewable source of liquid for extraction and a real-joint feel. To provide this source, students settled on Vitamin D capsules, which could be replaced easily and often.
Author/Photographer: Elizabeth Innes, Communications Specialist, I-STEM Education Initiative
More: BioE, Undergrad, 2012









.jpg)